13 min read
The Continuous Care Compass: Navigating Ongoing Health Services
 Sydney Giffen
:
Updated on February 17, 2026
Sydney Giffen
:
Updated on February 17, 2026

What Continuous Care Services Really Mean for You and Your Family

Continuous care services are specialized, short-term support designed to help people manage acute health crises at home, typically lasting only 2-3 days. These services bring skilled nursing care directly to the client during periods of severe symptoms—offering an alternative to hospital admission and helping families steer some of the most challenging moments in care.
Quick Definition:
- What it is: A Medicare-defined level of hospice care providing predominantly nursing support for at least 8 hours per day during a medical crisis
- Primary goal: Manage acute symptoms (pain, breathing difficulties, agitation) to keep clients comfortable at home
- Duration: Brief periods—usually just a few days—until symptoms stabilize
- Who provides it: Registered nurses, LPNs, and nursing aides working in coordinated shifts
- Where it happens: Wherever the client calls home—private residence, assisted living, or other supportive environments
When a loved one's health suddenly changes, the support landscape can feel overwhelming. You may hear providers mention different "levels of care" or discuss whether someone qualifies for "continuous care." In these stressful moments, clarity matters.
This guide explains what continuous care services are, when they're appropriate, and how they fit into the broader picture of support. We'll cover eligibility, billing, and practical realities so you can make informed decisions.
While continuous care addresses acute medical needs, many families also need ongoing, non-medical support for independence and quality of life. Understanding both helps you steer all available care options.
Basic continuous care services terms:
- aged care aides
- body hygiene in aged care
What is Continuous Care? A Closer Look at This Intensive Support

At its heart, continuous care services are a specific, intensive level of hospice support. It’s not an everyday service but a targeted intervention for acute needs—a specialized surge of support to bring comfort and stability during a health crisis. This guide explains what this entails.
This care is provided when a client experiences severe symptoms from a terminal illness that require frequent monitoring and intervention. The primary goal is to manage these acute symptoms effectively, ensuring the client remains comfortable at home and avoids a disruptive hospital admission. This short-term, acute care is a Medicare-defined level of hospice care, adhering to strict federal guidelines.
For families, this means a dedicated team can address urgent needs during a challenging period, offering reassurance and expertise. This allows them to focus on their loved one, not medical complexities. It’s about bringing care to the client, providing relief when it’s needed most. More info about our approach.
The Primary Goals of Continuous Care Services
When continuous care is initiated, several key objectives guide the hospice team's actions:
- Symptom relief and comfort: This is paramount. The primary aim is to alleviate severe and uncontrolled symptoms such as pain, breathing difficulties, nausea, vomiting, or agitation. The focus is on making the client as comfortable as possible.
- Managing pain and distress: Skilled interventions are deployed to bring acute pain and other forms of distress under control, often involving frequent medication adjustments and close monitoring.
- Supporting clients at home during a crisis: Continuous care is specifically designed to enable clients to remain in their own home or familiar care setting through a health crisis. It acts as a bridge, preventing the need for transfer to an inpatient facility or hospital.
- Providing skilled nursing presence: This level of care ensures that a registered nurse (RN), licensed practical nurse (LPN), or licensed vocational nurse (LVN) is present for a significant portion of the day to provide direct, hands-on medical care and observation.
- Offering reassurance and guidance to families: During a crisis, families often feel overwhelmed. The continuous presence of skilled professionals offers invaluable reassurance, education, and support, helping family members understand what is happening and how best to support their loved one.
Key Benefits for Clients and Families
The provision of continuous care services offers significant advantages during a critical time:
- Improved comfort and peace of mind: Knowing that skilled professionals are present to manage symptoms around the clock can greatly reduce anxiety for both the client and their family, fostering a sense of security.
- Reduced anxiety during difficult times: The presence of a dedicated care team helps to stabilize acute situations, reducing the stress and fear often associated with rapid health decline.
- Professional support on-site: Immediate access to professional medical expertise means that symptoms can be addressed promptly and effectively, often preventing escalation.
- Avoidance of hospital transfers: By managing acute symptoms at home, clients can avoid disruptive and often distressing transfers to hospitals or inpatient units, allowing them to remain in familiar, comforting surroundings.
- Empowerment for families to focus on connection: With medical needs being professionally managed, families are freed from the intense burden of caregiving during a crisis. This allows them to focus on emotional support, presence, and connection with their loved one.
The Four Levels of Hospice Care (Educational Context)
Understanding continuous care services requires placing it within the broader context of hospice care, which is structured into four distinct levels defined by Medicare. These levels ensure that clients receive the appropriate intensity of care based on their needs:
- Routine Home Care (RHC): This is the most common level of hospice care, involving intermittent visits from the hospice team (nurses, aides, social workers, chaplains) to the client's home. It focuses on ongoing symptom management, emotional support, and assistance with daily living, but does not involve continuous presence.
- Continuous Home Care (CHC): As we're exploring, this level provides intensive, short-term nursing care for acute symptom management during a crisis, typically in the client's home.
- General Inpatient Care (GIP): This level is provided in an inpatient facility (e.g., a hospital, hospice inpatient unit, or skilled nursing facility) when symptoms are so severe that they cannot be managed at home, even with continuous home care. It's for short-term crisis stabilization.
- Inpatient Respite Care (IRC): This provides temporary relief for primary caregivers, allowing the client to be cared for in an inpatient setting for up to five consecutive days. It's not for symptom management but purely for caregiver relief.
Here's a comparison between Routine Home Care and Continuous Home Care, highlighting their key differences:
| Feature | Routine Home Care (RHC) | Continuous Home Care (CHC) |
|---|---|---|
| Care Intensity | Intermittent visits by hospice team members | Intensive, acute care with significant skilled presence (min. 8 hours/day) |
| Primary Goal | Ongoing symptom management, support, and comfort | Short-term crisis intervention and acute symptom stabilization |
| Duration | Ongoing, as long as hospice eligibility criteria are met | Brief periods, typically 2-3 days, until symptoms are controlled |
| Staffing | Scheduled visits from RNs, LPNs, CNAs, social workers, etc. | Predominantly nursing care (RNs, LPNs, LVNs) with aide support, in shifts |
What Symptoms or Conditions Warrant Continuous Care?
Continuous care services are reserved for periods of crisis when a client's symptoms become acute and cannot be managed by routine hospice care or by the primary caregiver. These are situations where immediate, intensive medical intervention is needed to prevent hospitalization and provide comfort. Specific symptoms or conditions that often warrant continuous care include:
- Uncontrolled pain: When standard pain management strategies are no longer effective, and a client is experiencing severe, persistent pain.
- Severe nausea or vomiting: Intractable nausea and vomiting that cannot be controlled through routine medications, leading to significant discomfort and potential dehydration.
- Acute respiratory distress: Profound shortness of breath or other severe breathing difficulties requiring continuous monitoring and respiratory interventions.
- Agitation or restlessness: Extreme agitation, delirium, or restlessness that poses a risk to the client's safety or significantly impacts their comfort.
- Seizures: New onset or uncontrolled seizure activity requiring immediate medical management.
- Sudden decline requiring intensive nursing: Any rapid and significant change in a client's condition that necessitates continuous skilled observation and intervention to stabilize their symptoms and ensure comfort. This could include changes in consciousness or other acute medical issues.
How and Where is Continuous Care Provided?

One of the defining characteristics of continuous care services is that they are designed to be provided in the client's preferred environment. This means the care comes to them, allowing them to remain in familiar and comforting surroundings rather than being moved to an unfamiliar facility.
Where it happens: Continuous care can be provided wherever the client calls home. This commonly includes:
- A private residence.
- An assisted living community.
- A long-term care facility or nursing home.
The goal is always to help the client stay in place through a health crisis, rather than requiring a transfer elsewhere.
How it's provided: Continuous care is delivered by a hospice team working in shifts, ensuring a consistent presence during the crisis.
- Shifts and duration: Care is provided for at least 8 hours in a 24-hour period, which can be broken into smaller blocks. While it can extend up to 24 hours per day, it is not an ongoing 24-hour-a-day service. This intensive support usually lasts only two to three days, until the acute symptoms are brought under control.
- Predominantly nursing care: A core requirement is that the care provided must be predominantly nursing care, meaning at least 50 percent of the total care provided must be by a registered nurse (RN), licensed practical nurse (LPN), or licensed vocational nurse (LVN). Hospice aides or homemaker services can supplement this, assisting with activities of daily living (ADLs) and comfort measures. However, if aide hours exceed nursing hours, the day must be billed as routine home care, not continuous home care.
- Team collaboration: The hospice RN typically makes the initial assessment, coordinates the plan of care, and reassesses the client daily. LPNs provide bedside care, and CNAs assist with personal care and comfort. This team works collaboratively with any existing facility staff to ensure seamless support.
This approach ensures that during a brief but intense period, the client receives the highest level of skilled attention, focused entirely on symptom management and comfort in their chosen setting.
Navigating the Logistics of Continuous Care Services
While the clinical aspects of continuous care services are focused on client comfort, there's also a significant logistical and administrative side, particularly concerning Medicare and other payers. Understanding these aspects is crucial for both providers and families. The system is designed to ensure that care is provided appropriately and that providers are properly reimbursed for these intensive services.
Medicare Guidelines for Continuous Home Care
Medicare plays a central role in defining and covering continuous home care (CHC) within the hospice benefit. These guidelines are critical for ensuring appropriate use and billing:
- Crisis requirement for eligibility: CHC is explicitly designed for "periods of crisis to maintain the beneficiary at home." This means there must be an acute medical event or uncontrolled symptoms that necessitate intensive, short-term skilled care. It's not for general safety concerns or caregiver breakdown without acute symptom needs.
- 8-hour minimum rule: To qualify as a CHC day, an individual must receive at least 8 hours of hospice care within a 24-hour period (from midnight to midnight). If less than 8 hours of care is provided, or if the client passes away before 8 hours, the day cannot be billed as CHC and reverts to routine home care.
- Majority of care must be nursing (>50%): A cornerstone of CHC is that the care must be "predominantly nursing care." This means that more than 50% of the total aggregate hours provided in that 24-hour period must be delivered by an RN, LPN, or LVN. Homemaker or hospice aide services can contribute to the total 8 hours but cannot constitute the majority of the care. For instance, if a client receives 6 hours of aide care and 4 hours of nursing care, it would not qualify as CHC because nursing care is less than 50% of the total (10 hours).
- Billing in 15-minute increments: Hospice providers bill for CHC in 15-minute increments. This detailed tracking ensures accuracy and compliance with Medicare requirements. The daily CHC rate is divided by 24 hours to arrive at an hourly rate, which is then applied to the 15-minute units.
For comprehensive details on these guidelines, you can refer to the official Medicare Benefit Policy Manual.
Documentation and Billing Requirements
Accurate and thorough documentation is not just good practice; it's a non-negotiable requirement for continuous care services under Medicare. Without it, claims may be denied, impacting the hospice provider's ability to offer these vital services.
- Detailed clinical notes: Every intervention, observation, and client response must be carefully recorded. Best practice suggests documenting at least hourly during CHC to clearly demonstrate the ongoing need for intensive care.
- Documenting the crisis and interventions: The medical record must clearly articulate the specific crisis that necessitated CHC, the acute symptoms present, and the skilled nursing interventions provided to manage those symptoms. This includes medication administration, vital sign monitoring, wound care, and other skilled services.
- Updates to the plan of care: The client's plan of care must be updated to reflect the initiation of CHC, outlining the specific goals for symptom management, the interventions to be used, and the expected outcomes.
- Justifying medical necessity: All documentation must clearly support that the services were reasonable and necessary to address the crisis and maintain the client at home. This means showing why routine home care was insufficient and why continuous, predominantly nursing care was required.
- Changes in level of care: When a client transitions from CHC back to routine home care, the medical record must explicitly document the date, time, and reason for the change (e.g., "Client's pain is controlled, and caregiver is now able to manage needs; routine care to begin 1/3/YY at 7 a.m.").
For more detailed information on Medicare billing, the Medicare Claims Processing Manual is an essential resource.
Potential Challenges and Considerations
While invaluable, continuous care services come with their own set of challenges for hospice providers and families alike:
- Staffing availability for intensive shifts: Providing 8-24 hours of skilled care daily requires significant staffing resources. Hospices must ensure they have enough qualified nurses and aides to cover these intensive shifts, which can be particularly challenging during nursing shortages or in rural areas.
- Risk of claim denial if criteria aren’t met: Due to the strict Medicare guidelines, there's a risk of claims being denied if documentation is insufficient, if the 8-hour minimum isn't met, or if nursing care doesn't constitute the majority of hours. This places a burden on hospices to maintain rigorous compliance.
- Family stress during transitions: Even when continuous care is successful, the transition back to routine home care can be stressful for families. They may have become accustomed to the constant presence of a nurse and may feel anxious about managing care with less direct support.
- Moving back to routine support after a crisis: This transition requires careful planning and communication. The hospice team works to ensure that symptoms remain stable and that the family feels equipped and supported as the intensity of care decreases.
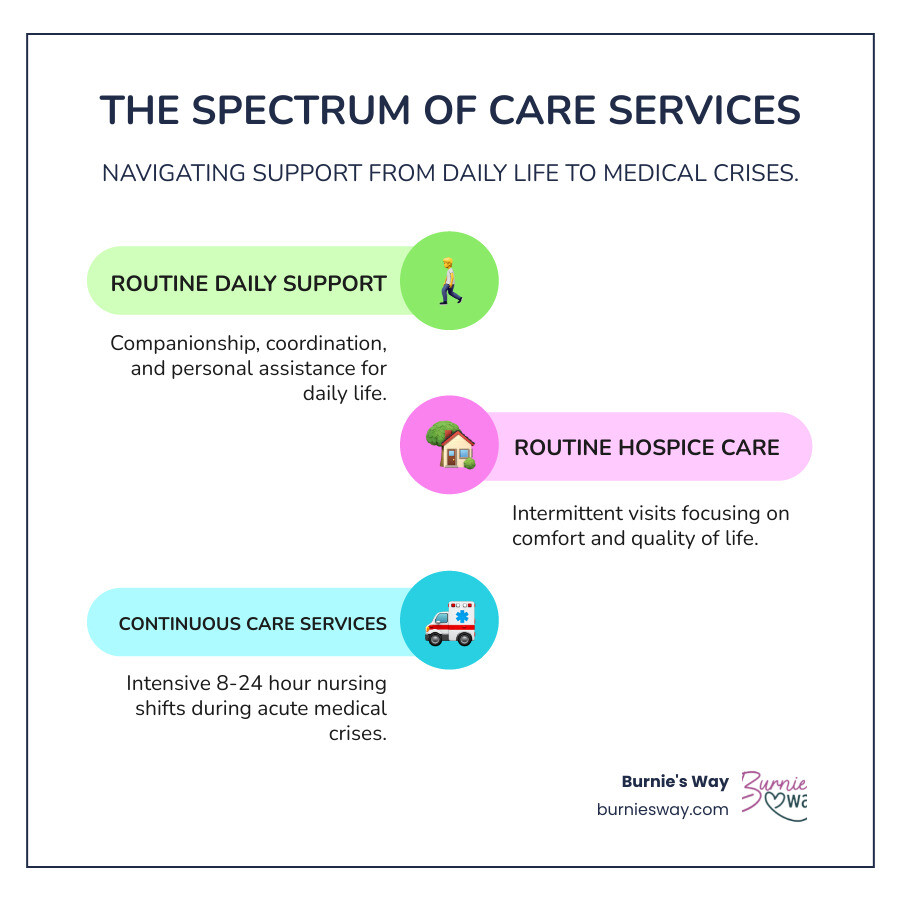
The Broader Spectrum of Ongoing Support
When we talk about "continuous care," it's easy to focus solely on the intensive, medical definition within hospice. However, the need for ongoing support extends far beyond medical crises. For many older adults and their families, "continuous support" means having help with the day-to-day rhythms of life, proactive planning, and ensuring independence and connection are maintained. This non-medical support is about enhancing quality of life, preventing isolation, and providing peace of mind for families.
Our lives are a mix of routines, social connections, and logistical demands. As we age, managing these aspects can become more challenging. That's where a broader spectrum of ongoing support comes into play. These services are not about acute medical interventions but about fostering a fulfilling and independent lifestyle.
Here are some different types of ongoing support that contribute to a comprehensive care ecosystem:
- Personal Support: Help with daily routines, organization, and maintaining a comfortable home environment.
- Social Support: Facilitating connections, engaging in hobbies, and combating loneliness.
- Logistical Support: Managing appointments, transportation, errands, and coordinating various services.
Continuous Care vs. Ongoing Personal Support (Educational Context)
It's crucial to distinguish between continuous care services (as defined by Medicare for hospice) and the broader concept of ongoing personal support. While both aim to provide comfort and stability, their purpose, duration, and nature are very different.
Continuous Care Services (Hospice):
- Focus: Acute medical symptom management during a crisis.
- Duration: Short-term, typically 2-3 days.
- Provided by: Medical professionals (RNs, LPNs, CNAs) delivering skilled care.
- Goal: Stabilize severe symptoms to avoid hospitalization and provide comfort in the client's final stages of life.
Ongoing Personal Support (Non-Medical):
- Focus: Daily life management, companionship, social engagement, and logistical coordination.
- Duration: Long-term, as needed to maintain independence and quality of life.
- Provided by: Non-medical professionals or personal concierges.
- Goal: Empower clients to live comfortably and confidently at home, maintain routines, stay connected, and manage everyday tasks.
Burnie's Way specializes in this latter category: providing ongoing personal support. We are not a caregiving or healthcare provider, and we do not offer medical continuous care services. Instead, we act as a personal concierge and trusted partner, helping our clients live the way they want, with support in key areas of daily life, and giving families peace of mind that everything’s okay. We provide the kind of help that bridges the gap between medical needs and a vibrant, independent life.
The Role of Non-Medical Continuous Support Services
Non-medical continuous support services are about enhancing life, not just managing illness. They are designed to be a proactive, consistent presence that helps individuals maintain their independence and enjoy their home life to the fullest. These services are especially vital when family members are geographically distant or juggling multiple responsibilities.
Our non-medical continuous support services focus on several key areas:
- Daily life management: Helping to organize household tasks, manage schedules, and ensure daily routines run smoothly. This could be anything from reminding clients about appointments to ensuring their pantry is stocked with their favorite snacks.
- Companionship and social connection: Combating loneliness and isolation through regular interaction, engaging in hobbies, or facilitating social outings. We believe in the power of connection and a good laugh!
- Coordination of appointments and activities: Managing a busy calendar of medical appointments (non-medical coordination), social engagements, and personal errands. We help keep everything on track so our clients don't miss a beat.
- Errand assistance: Taking care of shopping, picking up prescriptions (non-medical delivery), or other necessary errands that might be difficult for an individual to manage on their own.
- Proactive planning for routines and events: Helping to plan for upcoming events, holidays, or even just ensuring that daily routines are structured in a way that promotes well-being and reduces stress.
- Supporting independence and confidence: Our goal is to empower our clients. By handling the logistical burdens and providing consistent, friendly support, we help them feel more confident and capable in their own homes. It’s about helping them live life on their own terms.
This type of support is a testament to our commitment to helping individuals thrive at home. Our Story is rooted in understanding these diverse needs and providing solutions that truly make a difference in people's lives.
Frequently Asked Questions about Continuous Care
Here, we'll address some common questions to help clarify the specifics of continuous care services within hospice.
Is continuous care the same as 24/7 care?
This is a common point of confusion! While continuous care services can extend up to 24 hours per day if medically necessary, it is not automatically a round-the-clock service, nor is it an ongoing, permanent arrangement. Medicare guidelines specify that continuous home care requires a minimum of 8 hours of care in a 24-hour period. The care is provided in shifts and is specifically for brief periods of crisis. The intent is to stabilize acute symptoms, not to provide indefinite 24-hour personal attendance. Once the crisis is resolved, the client typically transitions back to routine hospice care, which involves intermittent visits.
Can a family request continuous care?
Families absolutely can and should communicate any sudden worsening of symptoms or acute distress to the hospice team. If a client's condition deteriorates to a point where routine care is insufficient, the family should report the crisis. The hospice clinical team will then conduct an assessment to determine if the client meets the strict medical criteria for continuous care services as defined by Medicare. While families can request an assessment, the decision to initiate continuous care is made by the hospice interdisciplinary team based on the client's acute medical symptoms and the necessity of skilled interventions. It's a medical determination, not simply a family preference.
How long does continuous care typically last?
Continuous care services are designed to be short-term. This level of care is intended for brief periods of crisis, usually lasting only two to three days. The duration is directly tied to the client's medical needs: it continues until the acute symptoms (like uncontrolled pain or severe respiratory distress) are brought under control and stabilized. Once the crisis has passed and the client's symptoms are manageable again with routine hospice interventions, they will transition back to routine home care. It is not meant to be a long-term solution for ongoing care needs.
Conclusion: Finding the Right Support for Every Stage
Navigating the complexities of health and aging can feel like charting unknown waters. Understanding continuous care services is a crucial part of this journey, especially when facing a medical crisis. We've seen that this is a specific, intensive level of hospice care, strictly defined by Medicare, designed to manage acute symptoms and keep a client comfortable at home during a short, critical period. It’s a vital service that provides skilled medical support when it's most urgently needed, helping to alleviate distress and prevent unnecessary hospitalizations.
However, the need for "continuous support" often extends far beyond these medical crises. For many older adults and their families, the desire to live independently and comfortably at home requires a different kind of continuous support—one that addresses daily life, social connection, and logistical coordination. This non-medical continuous support is about enriching life, maintaining routines, and providing peace of mind through proactive assistance and companionship.
At Burnie's Way, we specialize in providing this kind of personal, continuous support. We are not a medical care provider, nor do we offer hospice continuous care services. Instead, we act as your trusted partner and personal concierge, helping you or your loved one live confidently at home by managing the everyday details, fostering connections, and ensuring life runs smoothly. We believe that true independence is supported by a network of reliable, compassionate assistance. To learn how we can help you steer the ongoing support needed to thrive at home, we invite you to explore Our Services.

