Navigating Senior Care: A Planning Journey for Families
Why Planning Now Protects Independence Later Elderly care planning is the process of preparing for the support needs of aging adults before a...
13 min read
 Sydney Giffen
:
Updated on January 30, 2026
Sydney Giffen
:
Updated on January 30, 2026

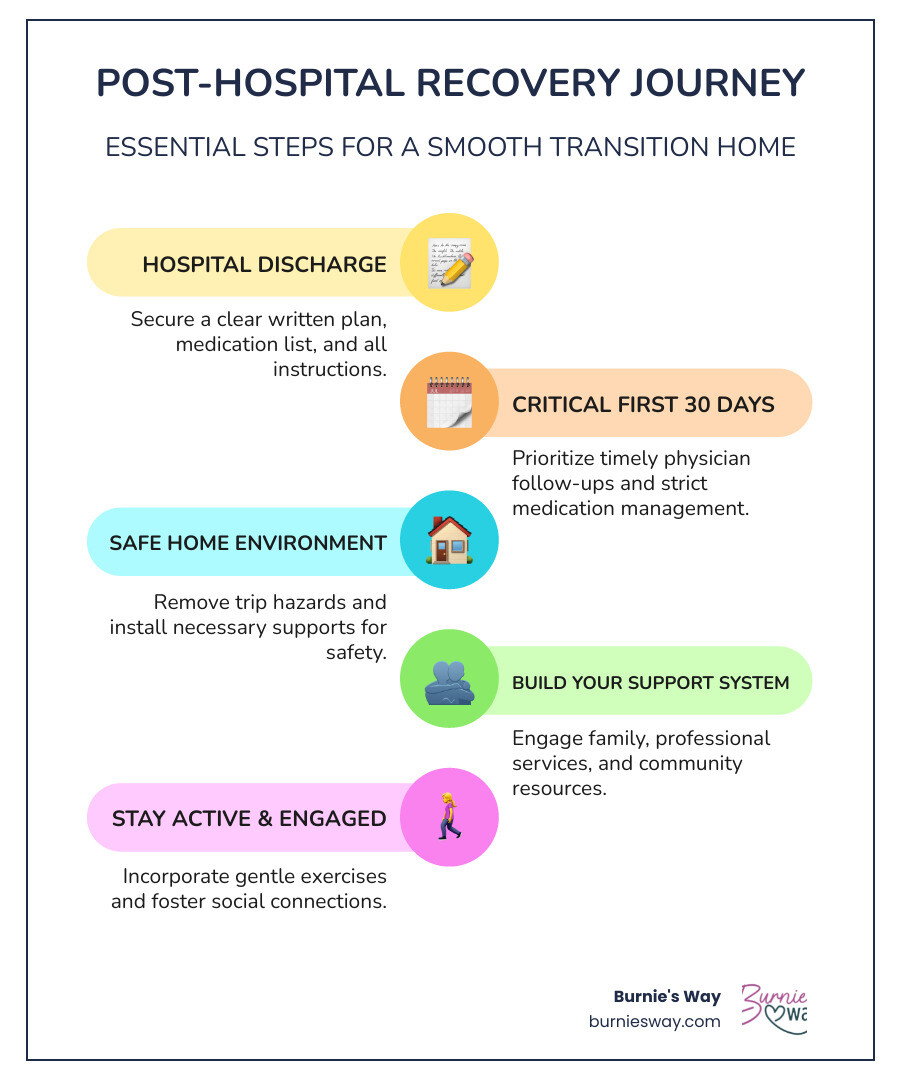
Post hospitalization care is the support and planning that helps you or your loved one safely transition from hospital to home—and it's crucial for preventing complications and readmission. Here's what you need to know:
Essential Elements of Post-Hospitalization Care:
Leaving the hospital is a major step forward in your health journey. But it can also feel overwhelming. After a serious illness that required you be in a hospital, leaving the hospital is your next step toward recovery—and a lot will change at this point.
The transition home is a vulnerable time. Around 35% of elderly patients are readmitted to the hospital within 90 days of being discharged. Many older adults are readmitted during the first month home—a period that requires careful attention and support.
The reason? Readmission often happens when patients don't follow doctor's instructions, struggle with medication schedules, or lack a proper recovery environment. Your body is under extra stress during hospitalization, and it takes time to get back to feeling better.
But here's the good news: proper planning makes all the difference. When you understand what to expect, create a clear care plan, and set up the right support systems, you dramatically improve your chances of a smooth, safe recovery at home.
This guide will walk you through everything you need to know about post-hospitalization care—from understanding the challenges you might face, to creating a solid discharge plan, to building the support system that helps you or your loved one heal with confidence and independence.
Quick look at post hospitalization care:
Coming home from the hospital can feel like a mixed bag of emotions. There's the relief of being in your own space, but often, that's coupled with a sense of vulnerability and uncertainty. For many, especially older adults, the journey back to full health after a hospital stay presents a unique set of challenges.

One of the most immediate challenges is often sheer physical weakness. Think about it: during bedrest, muscle loss happens quickly, with patients losing 2% to 5% of muscle mass for each day they are unable to walk. This rapid decline in strength can make even simple tasks like getting out of bed or walking to the bathroom feel like monumental efforts. Beyond muscle loss, patients might experience reduced circulation and general fatigue, making it hard to regain energy.
Emotional strain is another significant hurdle. Hospitalization itself is stressful, and the recovery period can bring anxiety, depression, or a feeling of isolation. Lingering symptoms from the illness, whether it's a persistent cough or a general feeling of being unwell, can contribute to this emotional toll.
For acute illnesses, the recovery journey can be particularly long and unpredictable. For example, after six months, over 70% of patients hospitalized for COVID-19 reported cardiopulmonary issues like cough, irregular heartbeat, or shortness of breath. Roughly half also experienced fatigue or physical limitations. This means that even after discharge, the battle isn't over; it's just shifted venues.
The period immediately following hospital discharge is often referred to as a "vulnerable transition point" for a good reason. The first 30 days at home following a hospitalization is a delicate time. Many older adults are readmitted to the hospital during this first month. This isn't just an unfortunate coincidence; it often stems from a lack of proper post hospitalization care.
Why do these readmissions occur? Often, it's due to an improper recovery environment or insufficient care oversight. Patients might struggle to stick to doctor's instructions, manage complex medication schedules, or simply lack the physical strength and support needed to heal effectively. Without a clear plan and consistent support, the risk of complications, falls, or worsening conditions increases significantly.
This highlights the immense importance of preparation and proactive support. Having a robust plan in place, and understanding how dedicated personal support can integrate with your recovery, can make all the difference during this critical window. We believe in empowering you to steer this period with confidence and ease. Learn more about our approach to supporting your daily life management.
The path to recovery is rarely a straight line, and the timeline can vary significantly depending on the illness and individual factors.
For acute illnesses like COVID-19 or pneumonia, recovery isn't always quick. As mentioned, many people hospitalized for COVID-19 should expect symptoms to last for up to six months or even longer, according to insights from Dr. Andrew J. Admon. With serious cases of pneumonia, recovery time can range from 6 to 12 weeks. While a general rule of thumb suggests one week of recovery for each day spent in the hospital, this is just an estimate.
Factors such as age, pre-existing conditions, and the severity of the illness all play a role in how quickly—or slowly—one recovers. A younger, healthier individual might bounce back faster than an older adult with multiple chronic conditions. Understanding these potential timelines helps set realistic expectations for both patients and their families, reinforcing the need for sustained support throughout the recovery journey.
The moment you leave the hospital is a pivotal point in your recovery. It's not just about walking out the door; it's about transitioning from a highly structured, medically supervised environment to your home, where you and your loved ones will take on more responsibility for your care. This is where a well-crafted discharge plan becomes your roadmap to success.
Discharge planning isn't a last-minute scramble; it's a collaborative process that ideally begins as soon as possible during your hospitalization. It involves you, your family or caregivers, and your entire hospital care team—doctors, nurses, social workers, and therapists. The goal is to ensure that when you leave, you have all the information, resources, and support you need to continue healing safely and effectively at home.
The Agency for Healthcare Research and Quality (AHRQ) emphasizes that effective discharge planning can help reduce medical errors during transitions of care, which is known to be a time during which patients are particularly vulnerable. You can find a comprehensive guide for leaving the hospital from AHRQ here.
This proactive approach, often guided by strategies like the IDEAL discharge planning model (which stands for Include, Discuss, Educate, Assess, Listen), focuses on patient and family engagement to ensure everyone is on the same page and feels prepared.
Before you or your loved one leaves the hospital, asking the right questions is paramount. This isn't the time to be shy! We encourage you to be a proactive advocate for your recovery. Here’s a list of essential questions to guide your conversations with the care team:
Remember to write down the answers or have a trusted family member take notes. It's a lot of information, and having it in writing will be incredibly helpful.
Your discharge plan isn't just a verbal conversation; it should be a tangible document that serves as your personal recovery guide. This written plan is formally known as a patient-oriented discharge summary (PODS) in some healthcare systems, and it's designed to empower you with clarity and confidence.
At a minimum, your discharge plan should include:
This comprehensive document is not just for you; share it with your family and any personal support professionals who will be assisting you. It ensures everyone involved in your post hospitalization care understands your needs and can support your journey back to independence. Having questions about the discharge process? We can help clarify common concerns. Check out our FAQ for more information.
The hospital's job is to treat your acute condition. Your home, however, is where the real healing often takes place. Navigating this journey effectively means optimizing your home environment, mastering medication management, and gradually re-engaging with physical activity and social connections. This holistic approach is key to a successful recovery.

Your home should be a sanctuary for recovery, not a source of new hazards. After an extended hospital stay, it may be some time before you regain your energy, balance, and coordination. To avoid trips, slips, and falls in your home, some smart precautions after recovery include:
Think of your home as a recovery zone. Small adjustments can make a huge difference in your safety and comfort, allowing you to focus on healing without unnecessary worries.
Medication management is often one of the most complex aspects of post hospitalization care. You might be on new medications, different dosages, or a completely revised schedule. Errors in medication can lead to serious complications and even readmission. Here’s how to manage it effectively:
Don't hesitate to ask your pharmacist questions; they are an invaluable resource for medication information and can help clarify any confusion.
While rest is crucial for recovery, prolonged inactivity can be detrimental. Muscle loss happens quickly during bedrest, with patients losing 2% to 5% of muscle mass for each day they are unable to walk. This can lead to further weakness, reduced mobility, and a longer recovery.
The goal is not just physical recovery, but also maintaining your overall well-being. A balanced approach that includes appropriate activity and social interaction will significantly contribute to a smoother and more fulfilling recovery.
Recovering from a hospital stay is rarely a solo endeavor. Building a strong support system around you is one of the most proactive steps you can take to ensure a full and lasting recovery. This network includes medical professionals, personal support services, and your community.
One of the most critical components of effective post hospitalization care is timely physician follow-up. The period immediately after discharge is a vulnerable one, and seeing your doctor promptly can prevent complications and adjust your treatment plan as needed.
We strongly encourage you to prioritize these follow-up appointments. If you need help finding local support resources or assistance with scheduling, many organizations can help. Explore support resources in your state.
When building your support system, it's helpful to understand the different types of professional services available. While Burnie's Way does not provide medical or in-home caregiving services, we can help you steer these options and coordinate the non-medical support that's right for you. Here are some common services you might encounter:
Understanding these distinctions is key. Burnie's Way acts as your personal support coordinator, focusing on lifestyle management and independence. Our role is to help you live comfortably at home by connecting you with trusted services and managing the routines that make life easier. We empower you to make informed choices about your care without providing the clinical or hands-on services ourselves. Find out more about how our flexible support plans are priced.
Beyond professional services, a robust personal and community support system is indispensable for post hospitalization care.
You don't have to steer this journey alone. Building a diverse network of support—from medical professionals to personal assistance, and from loved ones to community resources—will create a safety net that fosters healing and promotes long-term well-being. We are here to help you coordinate many aspects of this support system, allowing you to focus on your recovery. Get in touch with us to discuss your needs.
The journey back to health after a hospital stay can feel like a marathon, not a sprint. But with the right approach to post hospitalization care, it can also be a period of significant progress and renewed independence. We’ve explored the challenges—from physical weakness and emotional strain to the critical first 30 days—and highlighted the importance of a clear, comprehensive discharge plan.
By proactively engaging with your hospital care team, asking key questions, and understanding what to expect in your discharge instructions, you lay a strong foundation. Optimizing your home for safety and comfort, diligently managing medications, and gradually re-engaging with physical activity and social connections are all vital steps in this healing process.
Building a robust support system, including timely physician follow-ups and leveraging available professional and community resources, ensures you're never alone. We understand that navigating these complexities can be daunting, and that’s where our personal support comes in.
At Burnie's Way, we believe in empowering you to live safely and independently at home, especially during and after significant life events like a hospital stay. While we don't provide medical or caregiving services, we act as your personal support coordinator. Our role is to help you manage the non-medical aspects of daily life, connect you with trusted services, and coordinate routines that make your life easier and more enjoyable. We're here to help you live the way you want, with confidence and peace of mind.
Your recovery journey is unique, but the principles of good planning, active engagement, and a strong support network remain universal. By taking these proactive steps, you accept your healing journey with strength and optimism, paving the way for a return to a vibrant, independent life at home. Explore our personalized support services and discover how we can help you live confidently.

Why Planning Now Protects Independence Later Elderly care planning is the process of preparing for the support needs of aging adults before a...

Why Personal Support at Home Matters for Aging Adults Personal care for elderly at home includes essential daily activities that help seniors...

When Every Second Counts: Understanding Emergency Elderly Care Help